When to Start Sleep Training Baby: What Experts Suggest
We may earn a commission for purchases made using our links. Please see our disclosure to learn more.
It’s 2:17 a.m., you’ve done the feed, the burp, the rocking, the “please… just close your eyes” whisper-prayer… and your baby is still wide awake like they’re hosting a tiny midnight podcast.
If you’re Googling when to start sleep training baby, you’re not lazy, cold, or “doing it wrong.” You’re a tired human trying to help your baby (and your brain) get the rest you both deserve.
In this guide, we’ll talk about sleep training age, what “ready” actually looks like, gentle options (yes, they exist), how long it usually takes, and how to start in a way that feels solid—not scary.
The real reason this question feels so hard
Sleep training isn’t just a parenting task. It hits your emotions right in the softest spot.
Because it’s not really about sleep. It’s about:
- Your baby’s comfort
- Your peace of mind
- That deep fear of messing something up
And also… it’s about you needing rest to function like a person who can remember where they put their phone (spoiler: it’s in your hand).
So if you feel conflicted, that’s normal. You can love your baby fiercely and want longer stretches of sleep. Those two things can coexist.
What sleep training is (and what it isn’t)
Let’s simplify this.
Sleep training means helping your baby learn sleep skills—like falling asleep without being rocked all the way to “fully asleep,” and getting back to sleep after normal night wake-ups.
Sleep training is not:
- ignoring your baby’s needs
- refusing night feeds forever
- a one-size-fits-all “cry it out or nothing” situation
There are different approaches: gentle sleep training, graduated checks (Ferber-style), bedtime fading, and yes, cry-it-out (extinction). The best method is the one you can do consistently and emotionally tolerate.
When experts say most babies are ready
Here’s the helpful baseline: many babies are developmentally ready for more structured sleep training around 4–6 months.
Why? Because babies start developing more mature sleep cycles around this time, and routines tend to “stick” better. HealthyChildren.org (AAP) says that kids don’t sleep in regular patterns until they are roughly four months old.
That said, readiness isn’t a calendar date—it’s a combo of:
- age + development
- feeding/weight gain
- temperament
- your family situation
Important: If your baby was born premature or has reflux, breathing issues, or growth concerns, it’s smart to talk to your pediatrician before making changes.

Baby readiness signs you can spot at home
Instead of asking, “Is my baby old enough?” try asking, “Is my baby ready?”
Look for signs like:
- Baby is at least ~4 months and gaining weight steadily
- Night wakes feel more like habit than hunger (not always, but often)
- Baby can sometimes settle with a little support (not only full rocking/feeding)
- You’re seeing patterns: similar bedtimes, similar wake windows, predictable fussiness
- You can commit to a consistent plan for 7–14 days
A quick reality check
If your baby’s sleep is wildly chaotic right now, it doesn’t mean you failed. It may just mean your baby is still in that “newborn software update” phase.
When to pause: situations to talk to your pediatrician
Sometimes the best “sleep training plan” is… waiting a bit.
Consider pausing (or getting medical guidance) if:
- Baby is under 4 months
- Weight gain is a concern
- There’s significant reflux, eczema itching, chronic congestion, or suspected apnea
- You’re in the middle of illness, travel, or a major family change
- You’re struggling with postpartum anxiety/depression and the plan feels emotionally unsafe
This isn’t a moral judgment. It’s just timing.
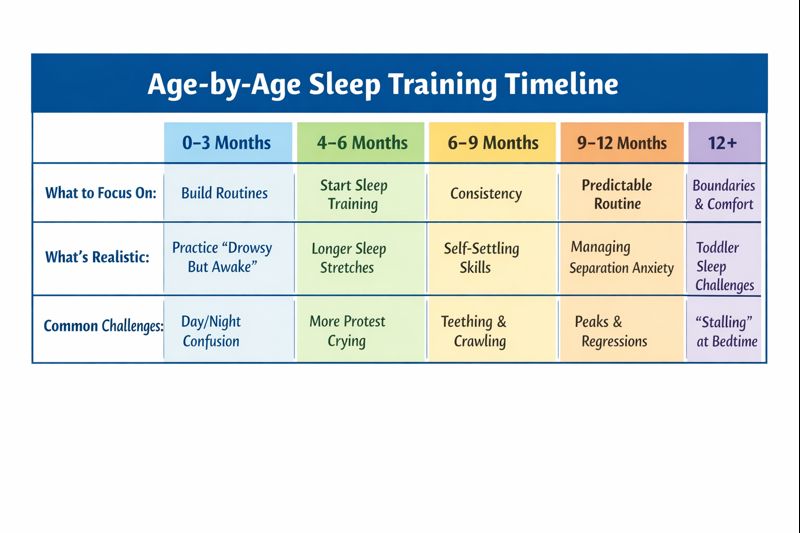
Age-by-age guide: 0–3, 4–6, 6–9, 9–12, 12+
Here’s the “road map” version—simple and realistic.
0–3 months: focus on foundations
You’re not training. You’re supporting.
- differentiate day vs night
- try a consistent bedtime routine (even 10 minutes counts)
- practice “drowsy but awake” gently (if it works, great—if not, no stress)
4–6 months: the classic starting window
This is when many families start structured sleep training.
- stronger bedtime routine
- consistent wake windows
- pick a method and stick with it
6–9 months: still a great time
If you skipped earlier, you didn’t miss the boat.
- baby may protest more (strong opinions arrive here)
- consistency matters even more
9–12 months: doable, but expect stamina training (for you)
- separation anxiety can spike
- routines need to be extra predictable
12+ months: more like toddler sleep coaching
- boundaries + routine + lots of consistency
- watch for “stall tactics” (yes, even babies start early)
Build a “sleep-friendly” setup first
Before you change how your baby falls asleep, set the stage.
Safe sleep basics matter most:
- Back to sleep
- Firm, flat surface
- No loose blankets/pillows/stuffed animals
- Room-sharing (not bed-sharing) is recommended for at least the first 6 months; AAP notes room-sharing can reduce SIDS risk significantly and is safer than bed-sharing.
Then add comfort helpers:
- dark room (or as dark as your home allows)
- steady white noise (optional, but helpful)
- comfortable temperature (not too warm)
If you’re wondering about clothing comfort, breathable fabrics can make bedtime less fussy—especially if your baby runs warm.

The bedtime routine that makes training easier
The bedtime routine is your secret weapon. It’s like telling your baby, “Okay, we’re powering down now.”
Keep it short and repeatable (20–30 minutes):
- feed (if applicable)
- diaper + pajamas
- calm activity (song, book, cuddle)
- into sleep space drowsy but awake (or awake-awake if that’s where you’re starting)
Pro tip: separate feeding from falling asleep
If baby always falls asleep while eating, that can become a sleep association. It’s normal, but if you want fewer wakes, try moving the feed earlier in the routine by 10–15 minutes.
Daytime basics: naps, wake windows, and feeding
This part is annoying because it’s true: day sleep affects night sleep.
If naps are all over the place, nights often get messier. Over-tired babies can fight sleep harder.
Helpful anchors:
- follow age-appropriate wake windows
- aim for consistent nap rhythm (even if naps aren’t long)
- keep daytime calories strong so nights aren’t purely hunger-driven
Also, sleep needs are real: the American Academy of Sleep Medicine consensus recommends 12–16 hours per 24 hours (including naps) for infants 4–12 months.
Pick your method: gentle, graduated checks, or full extinction
You’ve got options. Here’s a friendly overview.
Gentle sleep training (low-cry approaches)
Examples: pick-up/put-down, chair method, gradual fading.
- slower
- more hands-on
- great if crying is a major trigger for you
Graduated checks (Ferber-style)
You check at timed intervals, increasing gradually.
- often works within 1–2 weeks
- you’re present, but not “resetting” baby to fully asleep
Bedtime fading
You temporarily move bedtime later to build sleep pressure, then shift earlier.
- great for babies who fight bedtime
- often pairs well with consistent wake time
Full extinction (classic CIO)
No checks after bedtime (unless safety/needs arise).
- can be faster
- can be emotionally intense
No method is “the best” universally. The best method is the one you can do calmly and consistently.
What to expect the first 7 nights
Let me paint the honest picture.
Nights 1–2: “What is happening??”
Baby may protest because the routine changed. That’s not trauma—that’s confusion.
Nights 3–4: the extinction burst (sometimes)
Some babies fuss more right before improvement. This is common in behavior change.
Nights 5–7: you see patterns
You’re looking for:e “challenge” you’re asking for (bedtime first, then night wakes), and make sure baby’s basics are met (fed, comfortable, safe sleep space). You’re allowed to pick the approach that protects your nervous syste
- shorter time to fall asleep
- fewer/shorter night wakes
- easier settling after wakes
If you’re seeing any improvement, you’re on the right track.
Also, real-world timelines vary, but one pediatric sleep overview from University of Chicago Medicine notes some methods can work in a few days, while graduated approaches may take about a week or more.
Product Section: Helpful sleep training tools
Below are five practical, low-regret items parents often use to support a calmer bedtime routine. (Ratings/review counts change—always check the current listing.)
Hatch Rest Baby Sound Machine, Night Light & Time-to-Rise
Why it helps: Consistent white noise + a soothing light cue can become part of your bedtime “signal.”
Features: sound machine, night light, routines/timers (varies by model).
Best for: families who want one device to cover sound + light + routine cues.
Infant Optics DXR-8 PRO Video Baby Monitor
Why it helps: Sleep training is easier when you can check safety without constantly walking in.
Features: dedicated monitor, video feed, options vary by bundle.
Best for: parents who want a reliable monitor for nights and naps.
NICETOWN 100% Blackout Window Curtain Panels
Why it helps: Darkness supports melatonin and reduces early morning “sunrise parties.”
Features: blackout panels, insulation benefits depend on setup.
Best for: early-riser babies and bright rooms.
HALO SleepSack 100% Cotton Wearable Blanket
Why it helps: A wearable blanket keeps baby warm without loose bedding (safer sleep setup).
Features: cotton, zipper design, sizes vary.
Best for: babies who wake up cold or kick off blankets (which they shouldn’t have yet anyway).
Precious Little Sleep: A Comprehensive Guide to Baby Sleep for Modern Parents
Why it helps: You can feel less lost if you have clear explanations and useful tactics.
Features: evidence-informed approach, troubleshooting by age/stage.
Best for: parents who want a “tell me why this is happening” guide and what to do next.
Research-Backed Credibility: What science and experts say
Two helpful “zoomed-out” takeaways from research:
- Sleep training methods can improve sleep without showing long-term harm in some studies. A well-known randomized trial found graduated extinction and bedtime fading improved infant sleep, without evidence of adverse long-term effects in measured outcomes. Read: graduated extinction and bedtime fading study (Gradisar et al., 2016).
- Bigger-picture reviews also find behavioral sleep interventions can reduce night awakenings and improve parent sleep/well-being in many cases. Read: systematic review & meta-analysis on behavioral sleep interventions (Park et al., 2022).
And one comfort-related note: bedtime can go smoother when your baby isn’t itchy, sweaty, or overheated. If you want a quick guide to baby-friendly materials, here’s a helpful read: best fabrics for baby clothes (soft, breathable options).
FAQs about when to start sleep training baby
When to start sleep training baby if they’re waking every hour?
If your baby is under 4 months, focus on routine and sleep environment first. If they’re 4–6+ months, hourly wakes can be habit, discomfort, or feeding patterns—so start by tightening bedtime routine, optimizing naps, and choosing a method you can do consistently for 7–14 nights.
Is 4 months too early for sleep training?
Many families start around 4 months because sleep cycles mature around then.
Still, “ready” matters more than the exact birthday—especially if weight gain or medical issues are involved.
When to start sleep training baby who is breastfed?
Sleep training is definitely possible for breastfed infants. The key is separating feeding from falling asleep when possible and keeping night feeds that are still age-appropriate. If you’re unsure, a pediatrician can help you decide what’s normal for your baby’s growth and feeding needs.
How long does it take for sleep training to be effective?
Some families see change in 3–7 days, while others need 1–2 weeks, especially with gentler methods. Consistency is usually the biggest predictor of success.
What if sleep training makes my baby cry a lot?
Crying is communication, and change often triggers protest. If crying feels unbearable for you, choose a gentler method, shorten the “challenge” you’re asking for (bedtime first, then night wakes), and make sure baby’s basics are met (fed, comfortable, safe sleep space). You’re allowed to pick the approach that protects your nervous system too.




